Mental health is a critical part of overall wellness, and access to quality care is essential in order to live a full, healthy life. But many people are unaware of the coverage Medicaid provides for mental health services. Does Medicaid cover mental health? In this article, we’ll discuss the various types of mental health care Medicaid covers, and how to access these services.
Yes, Medicaid does cover mental health services. Medicaid is a government program that provides health insurance for people with low incomes, including those with mental health needs. Depending on the state, Medicaid can provide coverage for a range of mental health services, including counseling, medication, and inpatient and outpatient treatment.
Contents
- Does Medicaid Cover Mental Health Services?
- Individual and Group Therapy
- Top 6 Frequently Asked Questions
- What is Medicaid?
- Does Medicaid cover mental health?
- Who can receive Medicaid mental health coverage?
- What types of mental health services are covered?
- Are there limits to the amount of mental health services Medicaid will cover?
- Can private insurance and Medicaid be used together to pay for mental health services?
- Does Medicaid Cover Mental Health Care?
Does Medicaid Cover Mental Health Services?
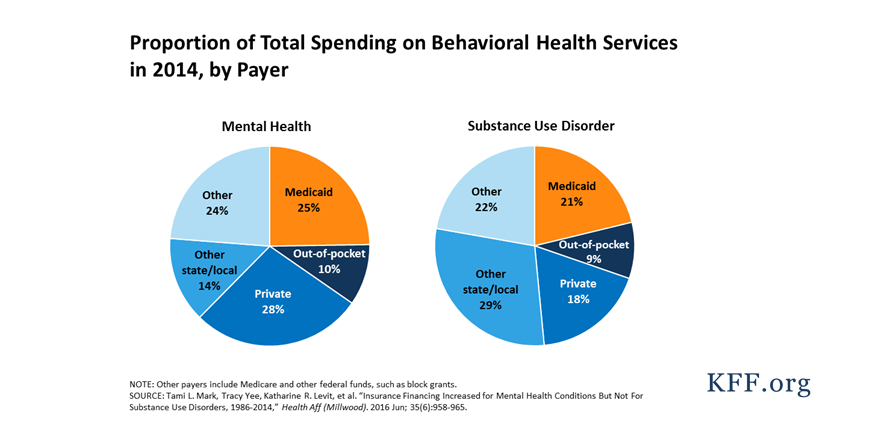
Medicaid is a government program that provides health insurance to people with low incomes and limited resources. The program is funded at both the federal and state levels, so coverage can vary from state to state. While Medicaid does not cover all mental health services, it does provide coverage for certain types of mental health care.
In general, Medicaid covers mental health services such as inpatient and outpatient care, individual and group therapy, medication management, and crisis services. The specifics of what is covered can vary depending on the state, so it is important to check with your local Medicaid office for the most up-to-date information.
In some cases, Medicaid may also cover additional services, such as case management, family therapy, substance abuse treatment, and support services. Some states also offer specialized programs for children and adolescents with mental health needs.
Inpatient Care
Inpatient care is when a person is admitted to a hospital or other inpatient facility for a specific mental health-related issue. This type of care is usually covered by Medicaid, although coverage may vary depending on the state. In some cases, Medicaid may also cover the cost of transportation to and from the facility.
Inpatient care may include a variety of services, such as medication management, individual and group therapy, and crisis intervention. It is important to note that Medicaid may not cover the full cost of inpatient care, and some states may require prior authorization before services can be provided.
Outpatient Care
Outpatient care is when a person receives mental health services from a provider in an outpatient setting, such as a doctor’s office or clinic. This type of care is usually covered by Medicaid, although coverage may vary depending on the state.
Outpatient care may include a variety of services, such as individual and group therapy, medication management, and crisis services. In some cases, Medicaid may also cover the cost of transportation to and from the provider. It is important to note that Medicaid may not cover the full cost of outpatient care, and some states may require prior authorization before services can be provided.
Individual and Group Therapy
Individual therapy is when a person meets with a mental health professional on a one-on-one basis to receive counseling or therapy. Group therapy is when a person meets with a mental health professional and a group of people to receive counseling or therapy. Medicaid typically covers both individual and group therapy, although coverage may vary depending on the state.
Individual and group therapy can be used to treat a variety of mental health conditions, such as depression, anxiety, and trauma. The specifics of what is covered by Medicaid can vary depending on the state, so it is important to check with your local Medicaid office for the most up-to-date information.
In some cases, Medicaid may also cover additional services, such as family therapy and support services.
Medication Management
Medication management is the process of managing medications prescribed for mental health conditions. This type of care is usually covered by Medicaid, although coverage may vary depending on the state. In some cases, Medicaid may also cover the cost of medications that are prescribed for mental health conditions.
Medication management can be used to treat a variety of mental health conditions, such as depression, anxiety, and bipolar disorder. The specifics of what is covered by Medicaid can vary depending on the state, so it is important to check with your local Medicaid office for the most up-to-date information.
Crisis Services
Crisis services are services that provide immediate help to people in a mental health crisis. This type of care is usually covered by Medicaid, although coverage may vary depending on the state. Crisis services may include a variety of services, such as crisis hotline numbers, mobile crisis teams, and crisis stabilization units.
Crisis services can be used to treat a variety of mental health conditions, such as depression, anxiety, and suicidal ideation. The specifics of what is covered by Medicaid can vary depending on the state, so it is important to check with your local Medicaid office for the most up-to-date information.
Top 6 Frequently Asked Questions
What is Medicaid?
Medicaid is a government-funded health insurance program for people in the United States with limited income and resources. It is funded jointly by the federal government and individual state governments. Medicaid is administered by individual states, and the services covered by the program vary from state to state.
Does Medicaid cover mental health?
Yes, Medicaid does cover mental health services. Mental health services may include counseling, therapy, medication management, and other services related to mental health and wellbeing. The specific services covered by Medicaid vary by state, but most states offer coverage for some mental health services.
Who can receive Medicaid mental health coverage?
In most states, Medicaid mental health coverage is available to people who meet the income and resource criteria and who are determined to be eligible for Medicaid services. Some states also require a diagnosis of a mental health disorder to be eligible for coverage, while others may provide coverage for mental health services regardless of diagnosis.
What types of mental health services are covered?
The specific types of mental health services that are covered by Medicaid vary by state. Generally, Medicaid covers services such as counseling, therapy, medication management, and other services related to mental health and wellbeing. Medicaid may also cover inpatient mental health treatment in some cases.
Are there limits to the amount of mental health services Medicaid will cover?
Yes, there are limits to the amount of mental health services Medicaid will cover. Each state sets its own limits on the amount of mental health services that Medicaid will cover. Generally, Medicaid will cover a certain number of sessions per year and/or a certain dollar amount for mental health services.
Can private insurance and Medicaid be used together to pay for mental health services?
Yes, in some cases, private insurance and Medicaid can be used together to pay for mental health services. This is known as “coordinated care” or “dual coverage,” and it is available in some states. It is important to check with your insurance provider to see if coordinated care is available in your state.
Does Medicaid Cover Mental Health Care?
In conclusion, Medicaid does cover mental health services, but coverage varies in different states. While some states may provide comprehensive coverage, others may only cover a few services. It is important to understand your state’s specific coverage before seeking mental health services. Additionally, it is important to remember that Medicaid is there to provide assistance to individuals who need it, and it is important to take advantage of the benefits it can provide.
